CASE STUDY 2
PLEXIFORM UNICYSTIC AMELOBLASTOMA
|
A 22-year-old male patient came to the institute with the chief complaint of pain and swelling in the left side of the face since 3 months. The swelling gradually increased to attain the present size. Patient also complained of a foul discharge in the mouth. On questioning, no other relevant symptoms were noted.
|
 |

|
|
| General examination: | |||
|
No abnormality detected. Extra-oral examination showed: 1. No asymmetry of the face. 2. Left submandibular lypmhadenitis. 3. Paraesthesia of left half of the lower lip was noted. 4. On inspection, a diffuse swelling was noticed over the left ramus of mandible. The swelling was confined in its extent over the left masseter muscle. The overlying skin was normal in appearance. 5. On palpation, swelling was soft to firm in consistency, non-tender and skin temperature was normal. Slight fluctuance could be elicited in certain areas.
|
|||
| Intra-oral examination: | |||
|
1. Midline
shift of mandible to the left. 2. All permanent teeth erupted except
tooth 38. Fairly good oral hygiene. Teeth 35, 36 and 37 exhibited
slight mobility; tooth 37 being lingually tilted. Further, there was
no response to electric pulp testing in these teeth. 3. A well-circumscribed
swelling was noted obliterating the left mandibular buccal vestibule
in the region of premolars and first molar. The overlying mucosa was
red in colour and the swelling was tender and fluctuant to palpation.
A bony margin could be palpated at the periphery. 4. The left retromolar
region showed accumulation of pus. On clearing the pus, a draining
sinus was noticed that expressed pus and blood on applying pressure
on the swelling. |
|||
|
|
 |
 |
|
| Aspiration & Cytology: |
|
Clear fluid was aspirated, from the fluctuant region of the swelling, which appeared brownish orange in colour. The fluid was analyzed for chemical composition. Chemistry of the aspirated fluid: pH=8; Sp.Gra.=1.015; Leukocytes=75 leu/Ál; Nitrogen=positive; Protein=500 mg/dl; Glucose=present; Ketone=negative; Urobilirubinogen=negative; Bilirubin=negative; Erythrocytes=250 ery/Ál. |
a |
 |
|
A smear was prepared of the fluid and subjected to cytological examination. Cytology Report read : 1.Epithelial cells: average size, polygonal, centrally placed small oval/round nucleus, pale staining cytoplasm. The over all appearance of the epithelial cells is normal. 2.Polymorphs are found in good number. 3.Erythrocytes are present. 4.There are thin strands, stained pink (blue sometimes ) resembling keratin flakes(but could be fibrous debris). 5.Other cellular debris is also present. |
||
|
|
||
| Top |
| Radiographic examination: |
|
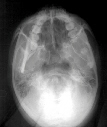
Radiographic Features: A large unilocular, homogenous radiolucent lesion in the left ramus and body of the mandible. The lesion occupied the entire ramus; obliterating the coronoid process and stopping short of the condylar neck. Anteriorly, it extended up to the root of the first premolar. Vertically, the lesion extended down to the inferior border of mandible and up into the alveolar process. The outline of the lesion was largely regular; with a little scalloping in some regions. |
||
 |
 |
 |
 |
The borders were partially hyperostotic and well-defined. The lesion had expanded in all directions causing thinning of the cortex anteriorly, inferiorly, lingually and buccally. The radiolucency appeared to be pericoronal to tooth 38, which was displaced to the angle of the mandible. Roots of teeth 35, 36 and 37 were resorbed; tooth 37 being lingually tilted. The inferior alveolar canal appeared displaced posteriorly and inferiorly. |
|
| Differential diagnosis: |
|
| Diagnosis: |
|
|
|
| Comments: |
|
Though the term ‘ameloblastoma’ was first suggested by Galippe in 1910, Ivy & Churchill were the first to encourage its usage in 1930. Generally speaking the ameloblastomas present at average age ranging from 33 years to 44 years, males being more frequently affected. The unicystic variety of ameloblastoma, however, shows a significant male preponderance and also, presents at an earlier age (2nd and 3rd decades). Not all unicystic ameloblastomas are plexiform in subtype. The plexiform unicystic variety typically contains a tooth and appears radiographically as dentigerous cyst. Most of them occur in mandible. Because of these features it is difficult to distinguish these tumors radiographically from odontogenic cysts. Microscopically, at least 75% of ameloblastomas are at least partially cystic; cyst formation ranging from microcysts to completely cystic tumor. Plexiform ameloblastomas typically show strands of ameloblast-like cells surrounding stellate reticulum-like cells in loose, vascular, sparsely cellular connective tissue. The recurrence rate of this distinct subtype is lower than other subtypes of ameloblastoma. |
| Top |
